Comprehensive Understanding of the Intersection of Mental Illness and Substance Abuse
The relationship between mental health and substance use is profoundly intertwined. When an individual experiences both a mental health disorder and a substance use disorder simultaneously, it’s known as “dual diagnosis” or “co-occurring disorders.”This complex condition presents unique challenges in diagnosis and treatment, often exacerbating symptoms of both conditions. This article delves into the intricacies of dual diagnosis, its far-reaching implications, and the critical importance of comprehensive, integrated treatment approaches.
What Exactly is Dual Diagnosis?
Dual diagnosis describes the presence of both a mental health illness—such as depression, anxiety disorders, bipolar disorder, schizophrenia, or post-traumatic stress disorder (PTSD)—and an addiction to drugs or alcohol. This overlap is more common than many realize, with leading health authorities showing that approximately 50% of individuals experiencing a mental illness also having a substance use problem, and vice versa.
The convergence of these disorders complicates the clinical picture significantly. Symptoms of one condition can mask or intensify the symptoms of the other, making accurate diagnosis challenging.For instance, someone with anxiety might turn to alcohol for temporary relief, but chronic drinking can worsen anxiety symptoms, creating a vicious cycle of deterioration.Conversely, substance abuse can induce symptoms that mimic mental illness, or even unmask a pre-existing genetic predisposition to a mental disorder.
Contact WeDoRecover to get help now.
Going Deeper: What Families Need to Know About Dual Diagnosis
Understanding the basics of dual diagnosis is vital—but if you’re supporting a loved one, it’s equally important to grasp what makes treatment effective, what to expect in the South African system, and why not all “integrated care” is created equal.
Why Dual Diagnosis Deserves Urgent, Evidence-Based Attention
While dual diagnosis is more common than many realise, it’s also far more serious. Research from the National Institute on Drug Abuse (NIDA) shows that nearly 50% of people with a substance use disorder also experience a mental health condition such as depression, anxiety, PTSD, or bipolar disorder. These conditions don’t just co-exist—they intensify one another, often making recovery far more difficult if treated in isolation. People with untreated co-occurring disorders are:
More likely to relapse after initial treatment
More prone to hospitalisation or emergency interventions
At higher risk of suicide and self-harm
More likely to experience long-term disability or job loss
In South Africa, these outcomes are often compounded by delayed access to care, stigma around mental illness, and limitations in the public mental health system.
South African Reality: Limited Access to True Integrated Care
While many South African rehabs claim to treat co-occurring disorders, true dual diagnosis treatment remains limited outside of select private facilities. A 2018 study led by Prof. Bronwyn Myers found that many treatment centres—especially those reliant on state funding—lack the resources, psychiatric personnel, or interdisciplinary collaboration to provide fully integrated care. This often results in a “parallel treatment” model where addiction and mental health are addressed separately (or not at all), leading to higher dropout rates and poorer long-term outcomes.
Even in the private sector, not all facilities are created equal. It’s important to look for:
Programmes that offer on-site psychiatric care
Staff trained in both mental health and addiction (not one or the other)
Consistent trauma-informed therapy (many co-occurring cases involve unresolved trauma)
Individualised care plans that treat the person, not just the diagnosis
If you’re considering treatment for a loved one in South Africa, ask specifically about how mental health conditions are assessed, monitored, and integrated into daily therapeutic work.
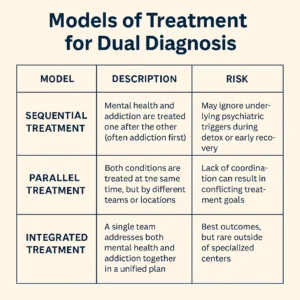
Not All ‘Integrated Treatment’ Is the Same
The phrase “integrated care” is often used in marketing—but there are actually several distinct models of treatment for dual diagnosis. Understanding the difference can help you choose the right programme:
| Model | Description | Risk |
|---|---|---|
| Sequential treatment | Mental health and addiction are treated one after the other (often addiction first). | May ignore underlying psychiatric triggers during detox or early recovery. |
| Parallel treatment | Both conditions are treated at the same time, but by different teams or locations. | Lack of coordination can result in conflicting treatment goals. |
| Integrated treatment | A single team addresses both mental health and addiction together in a unified plan. | Best outcomes, but rare outside of specialised centres. |
According to Dr. Kenneth Minkoff, a pioneer in dual diagnosis treatment, truly integrated care remains the gold standard—especially for individuals with severe or chronic mental illness alongside addiction. Minkoff, K. (2001). Developing standards of care for individuals with co-occurring psychiatric and substance use disorders. Psychiatric Services.
The Intricacies and Contributing Factors of Dual Diagnosis
The development of dual diagnosis is multifaceted, often stemming from a combination of genetic, environmental, and developmental factors:
- Genetic Vulnerabilities: A family history of either mental illness or substance use disorders can increase an individual’s susceptibility to developing both. Substance exposure itself can epigenetically activate genes associated with mental illness.
- Trauma and Stress: Early exposure to trauma, chronic stress, or abuse can significantly increase the risk for both substance use disorders and mental health conditions.
- Self-Medication: Many individuals use substances as a maladaptive coping mechanism to alleviate distressing symptoms of an untreated mental health disorder. While providing temporary relief, this often leads to worsening symptoms and dependence.
- Brain Changes: Substance use can alter brain chemistry and structure, potentially inducing mental health issues or exacerbating existing ones. The adolescent brain, still developing, is particularly vulnerable to these changes.
Common Co-Occurring Disorders
Beyond the general categories, specific mental health disorders frequently co-occur with substance use disorders:
- Anxiety Disorders: Generalized anxiety disorder, panic disorder, and social anxiety are commonly seen alongside substance abuse.
- Mood Disorders: Major depressive disorder and bipolar disorder have strong bidirectional links with addiction.
- Schizophrenia: Individuals with schizophrenia have a significantly higher prevalence of substance use disorders, which can worsen psychotic symptoms and impede treatment.
- Post-Traumatic Stress Disorder (PTSD): There’s a strong correlation, where individuals often use substances to cope with traumatic memories and hyperarousal.
- Personality Disorders: Antisocial personality disorder and borderline personality disorder are often comorbid with substance use disorders, contributing to complex treatment needs.
- Attention-Deficit Hyperactivity Disorder (ADHD): Impulsivity and difficulty with emotional regulation in ADHD can increase the risk of substance abuse.
Why Dual Diagnosis is Often Missed or Misdiagnosed
The overlapping nature of symptoms presents a significant diagnostic challenge. Clinicians may struggle to differentiate between substance-induced symptoms and those of an independent mental illness. Historically, mental health and addiction treatment systems operated separately, leading to fragmented care where one condition might be treated while the other was overlooked or exacerbated. Stigma associated with both conditions also acts as a barrier, deterring individuals from seeking comprehensive help.
The Imperative of Integrated Treatment
Addressing dual diagnosis effectively requires a holistic, integrated approach that treats both the mental health disorder and the substance use issue concurrently by the same team or program. This contrasts with traditional sequential or parallel treatments, which have proven less effective. Integrated care models offer several advantages:
- Coordinated Care: Ensures that treatment for one condition does not undermine the other, providing consistent explanations of illness and coherent treatment plans.
- Improved Outcomes: Studies consistently show that integrated treatment leads to better outcomes, including reduced substance use, fewer hospitalizations, improved mental health symptoms, greater housing stability, and enhanced functional status.
- Addresses Underlying Issues: Allows for a deeper exploration of the root causes of both conditions, such as trauma or maladaptive coping mechanisms.
- Reduces Relapse Risk: By treating both conditions simultaneously, individuals develop a more robust set of coping skills and a stronger foundation for long-term recovery.
- Studies consistently show that integrated treatment leads to better outcomes.
Key Components of Integrated Dual Diagnosis Treatment
Effective integrated treatment programs often incorporate a blend of pharmacological, psychological, and psychosocial interventions tailored to the individual’s needs:
- Detoxification and Withdrawal Management: Safely managing physical dependence on substances.
- Pharmacological Treatment: Medications to address mental health symptoms (e.g., antidepressants, mood stabilizers, antipsychotics) and reduce cravings or manage withdrawal from substances.
- Therapeutic Interventions:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change harmful thought patterns and behaviors that contribute to substance use and mental health symptoms.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, particularly beneficial for individuals with co-occurring mood or personality disorders.
- Trauma-Focused Therapy: Addresses underlying trauma that may contribute to both conditions.
- Motivational Interviewing: Enhances an individual’s motivation to change their substance use behaviors.
- Family Therapy: Involves family members in the recovery process, improving communication and support systems.
- Psychoeducation: Educating individuals and their families about dual diagnosis, its dynamics, and the recovery process.
- Life Skills Training: Developing healthy coping strategies, stress management techniques, and relapse prevention skills.
- Support Groups: Encouraging participation in peer support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) alongside mental health support groups.
- Long-Term Support: Recovery is an ongoing journey. Integrated programs often provide assertive outreach, case management, and sustained support to help individuals maintain stability and build a fulfilling life post-treatment.
The Path to Recovery
Navigating the complexities of dual diagnosis can seem daunting, but with the right support and integrated treatment, sustained recovery is well within reach. Learn more about the importance of comprehensive treatment and how that plays a crucial role in guiding individuals to make informed decisions about their rehab process, ensuring they receive the specialized, integrated care necessary for a dual diagnosis.
As awareness and understanding of dual diagnosis continue to grow, so do the resources and facilities dedicated to assisting individuals in reclaiming control of their lives and building a foundation for lasting well-being.
FAQs on Dual Diagnosis
- Is dual diagnosis common?
- Yes, it’s more common than you might think. Many individuals with a substance use disorder also suffer from a mental health disorder and vice versa.
- Which comes first: addiction or mental illness?
- It varies. Some may develop a substance abuse problem first, while others might have pre-existing mental health issues that lead to substance use as a coping mechanism.
- Why is dual diagnosis often missed or misdiagnosed?
- The overlapping symptoms can make it challenging to differentiate between the two disorders, leading to an incomplete diagnosis.
- Can dual diagnosis be treated?
- Absolutely. However, it requires a comprehensive approach that addresses both the mental health disorder and the substance abuse issue.
- Is specialised treatment necessary for dual diagnosis?
- Yes. Treating both conditions simultaneously is fundamental for effective recovery. Integrated interventions that cater to both the mental illness and the addiction offer the best outcomes.
- Is dual diagnosis treatment different from regular addiction treatment?
- Yes, dual diagnosis demands an integrated approach that simultaneously addresses both the mental health disorder and substance abuse. Centers like those in Johannesburg and Cape Town specialise in such treatments.
- How prevalent is dual diagnosis?
- Increasingly common, many individuals battling addiction also suffer from an underlying mental health disorder, necessitating specialised addiction treatment.
- What factors contribute to dual diagnosis?
- Genetics, trauma and environmental factors can all play a role in the onset of both substance abuse and mental health disorders.
- Are there specialised rehab centers for dual diagnosis?
- How effective is dual diagnosis treatment?
- With an integrated approach that addresses both conditions concurrently, many individuals experience significant improvement and lead fulfilling lives post-treatment.
Interesting Facts About Dual Diagnosis
- The link between mental illness and substance abuse isn’t coincidental. Some individuals use drugs or alcohol as a way to self-medicate, hoping to alleviate the symptoms of their mental health disorder.
- Dual diagnosis can sometimes lead to a vicious cycle where the untreated mental illness exacerbates substance abuse, which in turn aggravates the mental health symptoms.
- Research has indicated that individuals with dual diagnosis are more likely to experience homelessness, incarceration and significant medical illnesses.
Choosing the right rehab is essential for individuals with a dual diagnosis. Comprehensive centers that offer a blend of psychiatric care and addiction treatments are often the most effective. Places like WeDoRecover guide individuals in making informed decisions about their rehab process, ensuring they receive the integrated care necessary for a dual diagnosis.
A deeper understanding of the rehab process allows individuals to better grasp the path ahead. This process often starts with detoxification and transitions into therapeutic interventions tailored for both the mental health disorder and the addiction.
Exploring Rehabilitation Options
Rehab centers across South Africa, including those in Mpumalanga and the Garden Route, have started offering specialised programs catering to dual diagnosis. These centers recognise the unique challenges posed by dual diagnosis and have thus developed programs that holistically address both mental health and addiction.
Navigating the labyrinth of dual diagnosis might seem daunting but with the right support and integrated treatment, recovery is well within reach. As awareness and understanding grow, so do the resources and facilities dedicated to assisting individuals in reclaiming control of their lives.
Only 1 in 10 people
struggling with substance abuse receive any kind of treatment.Get help with evidence-based treatment today.
At We Do Recover, we're grounded in the belief that to overcoming addiction issues starts with something as simple as a phone call, email or an online chat with us. Our team, has vast experience as addiction counsellors and interventionists, is ready to offer you the support you need right from the start. Our core mission? To provide you with clear, direct help, ensuring you and your loved ones steer clear of treatments that don’t work and find the effective support you deserve. We know all too well how pressing the need is to confront the growing challenges of addiction and how crucial it is to reach out sooner rather than later. Through our blend of personal touch and professional expertise, we’ve guided countless individuals on the path to recovery and we can help you too.
Common Terms Used in Addiction Rehabs
Rehabs in other cities of South Africa.